Anatomy
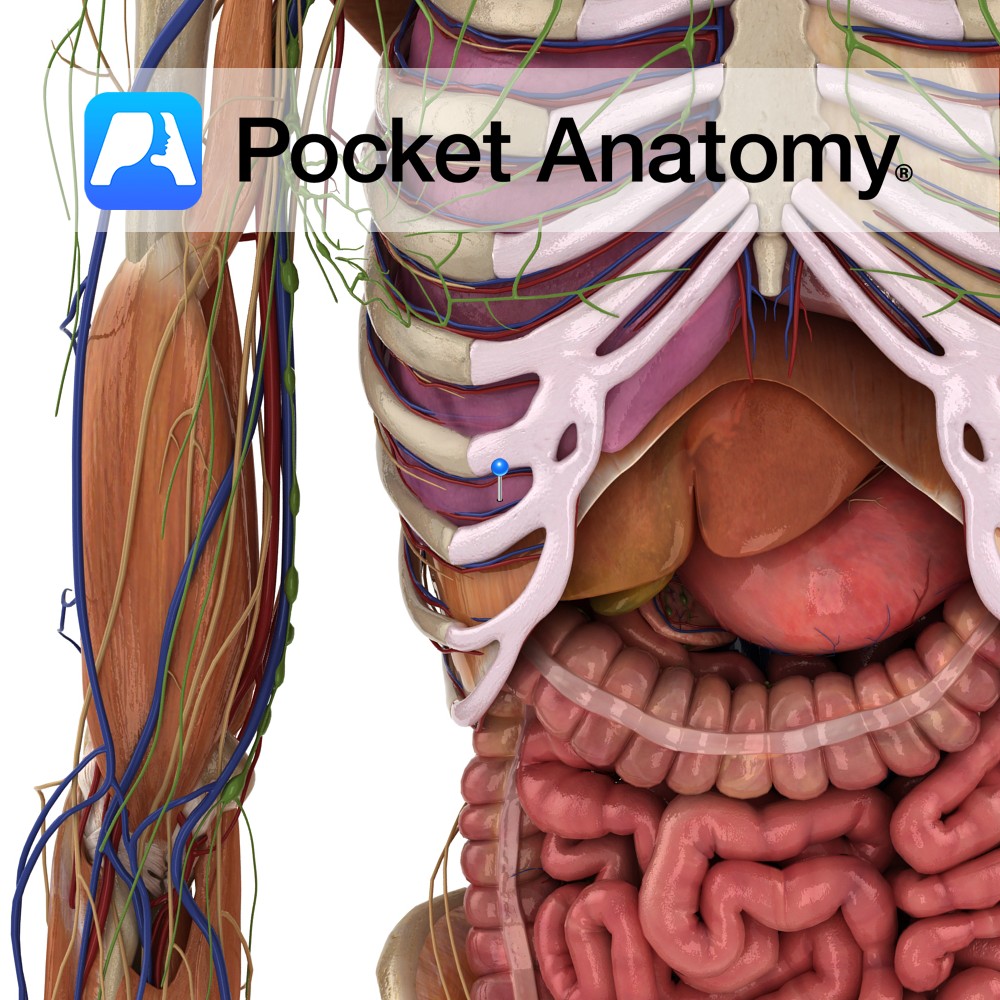
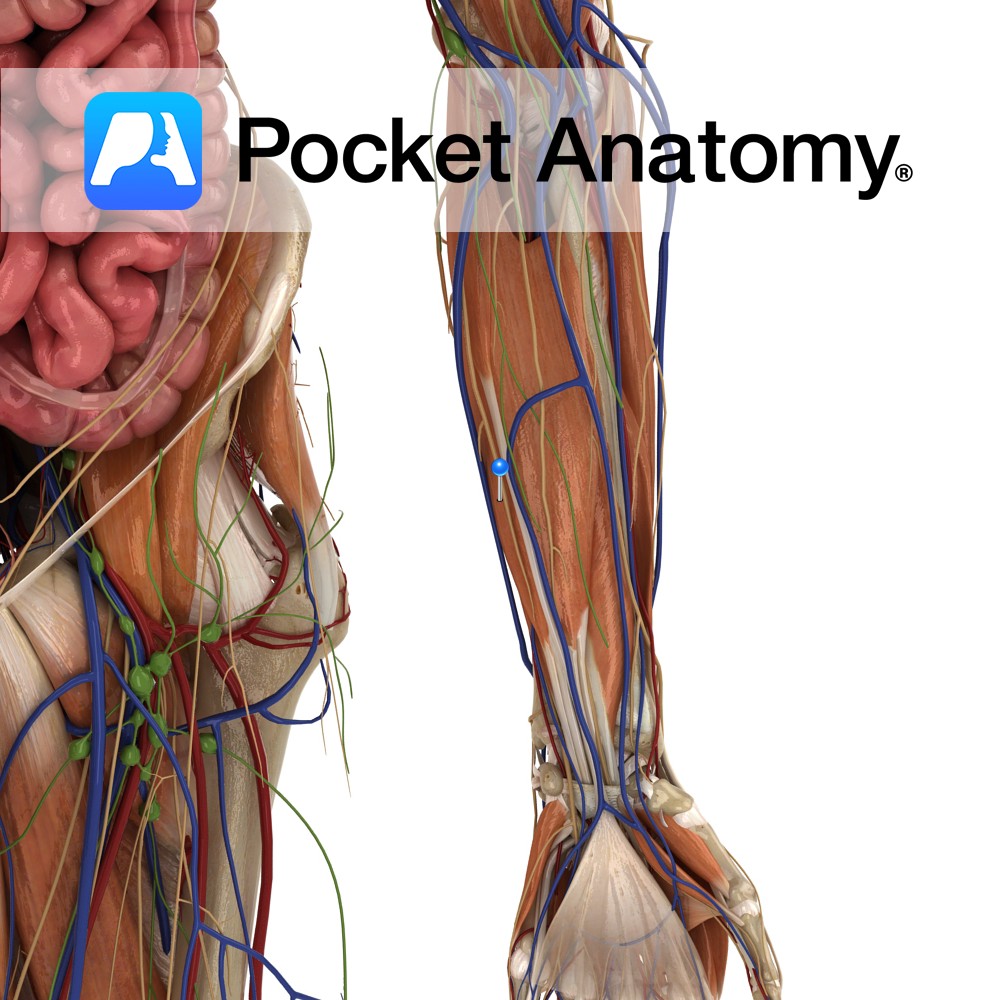
Two layered membrane in thorax, folded on itself like a deflated but tied balloon, ie there is a potential cavity (if it were re-inflated). Between the pleural layers is a small amount of lubricant fluid that allows touching sides to slide over each other.
One side (parietal – sensitive to pain) is externally attached to the inside of the thoracic wall and top of diaphragm, the other (visceral) is externally attached to the outside of the lung.
Thus, when the chest wall moves out and the diaphragm down, the elastic lung is expanded through suction, pulmonary pressure drops, and air enters passively.
Pleural cavity
Thin, potential space between visceral and parietal plurae, filled with pleural fluid (produced by intercostal arteries and reabsorbed by lymphatic system). Typically only a few millimetres of fluid is present. More (or less) leads to pathology.
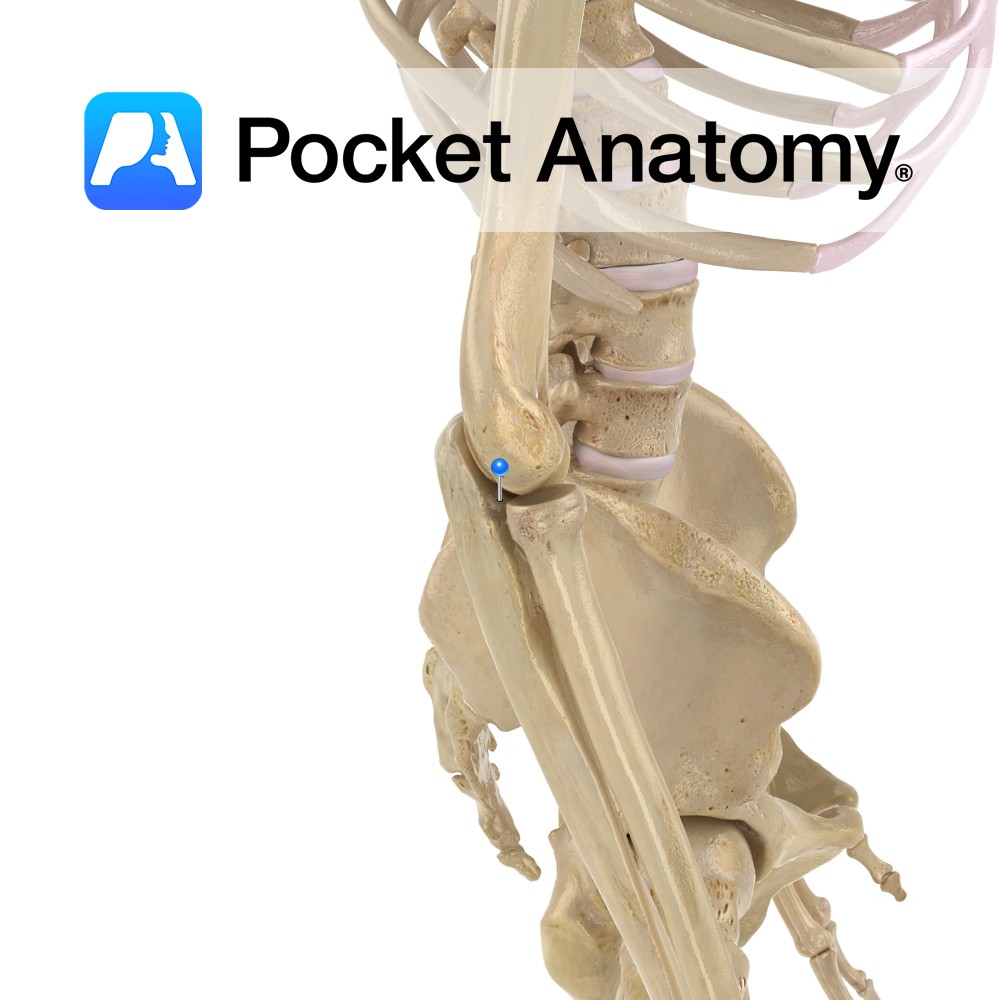
Develops from intraembryonic coelom in fetus, from the area between splanchnopleura (visceral pleura) and somatopleura (parietal pleura).
Functions: Assists in respiration. As the diaphragm descends it pulls on the parietal pleura, creating a negative pressure is created between the pleuras, causing the visceral pleura to pull and expand the lungs.
Visceral pleura
Delicate, thin, serous membrane that attaches directly to the lungs. Separated from parietal pleura by pleural cavity. Covers all the lung except a small area at the hilum.
Innervated by the pulmonary plexus.
Parietal pleura
Lines the inner thoracic wall, covers the superior surface of the diaphragm and separates pleural cavity from the mediastinum. The costal portion of the parietal pleura lines the inside of the ribs and intercostal muscles, though separated from them by endothoracic fascia. Various portions of parietal pleura are named depending on their area: cervical, costal, diaphragmatic or mediastinal pleura.
Innervated by intercostal nerves anteriorly, phrenic nerve inferiorly.
Functions
Assists in respiration. As the diaphragm descends it pulls on the parietal pleura, creating a negative pressure is created between the pleuras, causing the visceral pleura to pull and expand the lungs.
Clinical
Pleural cavity
Only a few millimetres of parietal fluid should exist (0.26 ± 0.1 mL/Kg); pathology occurs with excess fluid (pleural effusion) or when air (pneumothorax) or blood (haemothorax) enters. There is no connection between left and right cavities, so one lung will be spared if trauma occurs to the other.
Visceral pleura
Innervation, feeling. Inflammation is called ‘pleurisy’. Due to the nerve supply, it is sensitive to stretch but not pain and touch (as opposed to parietal pleura).
Parietal pleura
Senses pain, but visceral pleura does not. Therefore, chest pain on forced respiration would come from parietal pleura, not visceral pleura.
Interested in taking our award-winning Pocket Anatomy app for a test drive?