Anatomy
Cylindrical male external sexual organ (also serving as a urinal duct) through which sperm are extruded/ejaculated and introduced into the female vagina (during copulation/coitus/intercourse), from where they try (the attrition rate is well over 99.99%) to travel on and seek out an egg to fertilise. Size at any time influenced by factors such as arousal, temperature, time of day; tumescence (degree of size and rigidity) varies from flaccid (softest, smallest) to erect (hardest, largest – about 5-6″ long, diameter 1.5″).
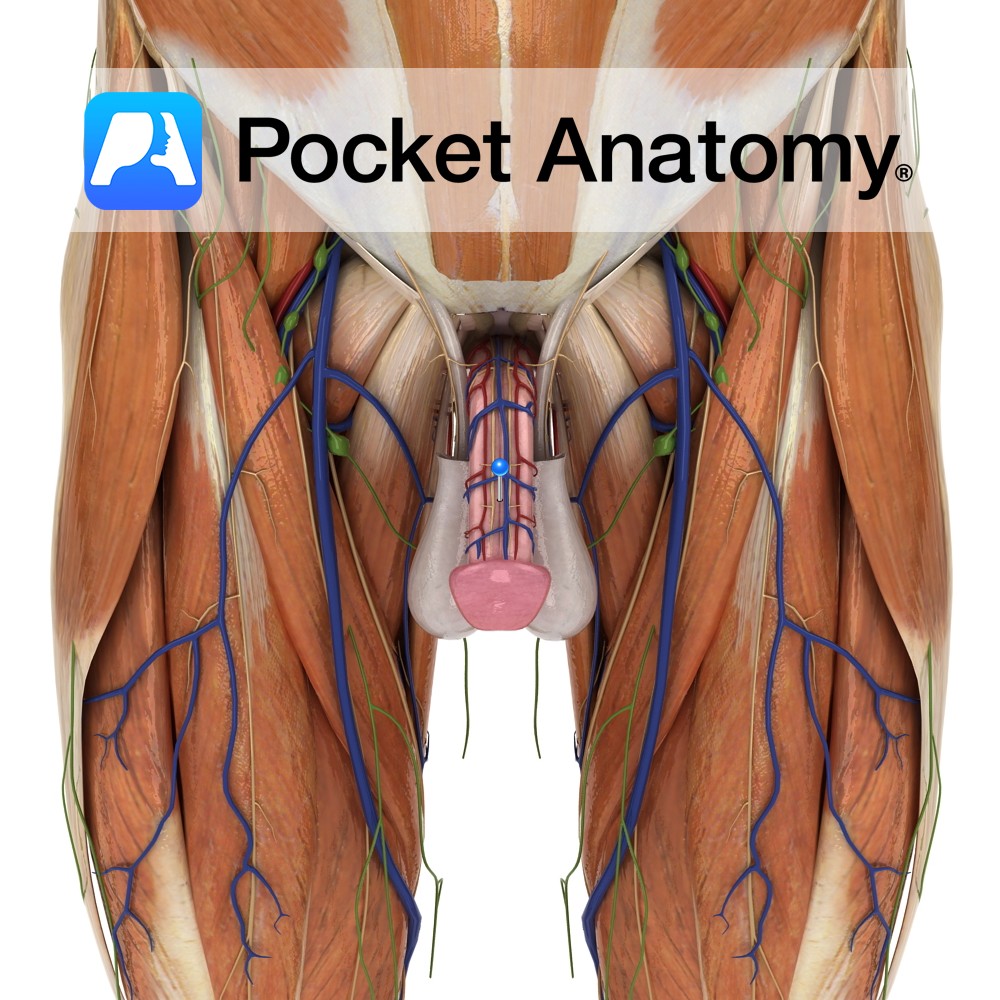
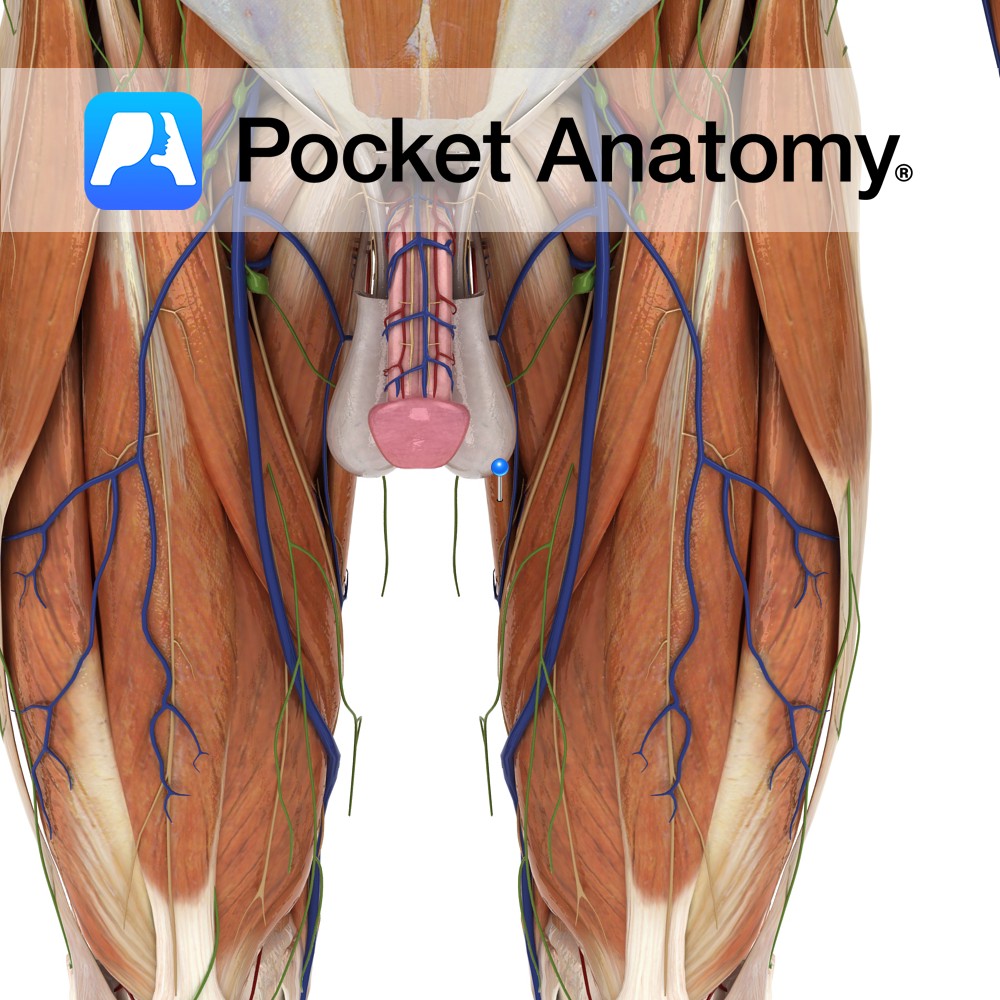
Penis has root (crus, either side of bulb, in superficial perineal pouch) and body (shaft and glans). Body covered with epithelium; skin on shaft and foreskin/prepuce (removed in circumcision), mucosa on inside of foreskin and on glans (female equivalent – clitoris).
Structures under epithelium; corpus cavernosum (paired, covered in 2 layers fascia) either side of and dorsal (the aspect furthest from the scrotum) to corpus spongiosum (ventral, covered in tunica albuginea, and through which spongy/anterior urethra passes), bulbous end of which is glans (at tip of which is meatus, the end and external opening of urethra).
Erection mediated by autonomic motor and somatic sensory nerves. Parasympathetic fibres (S2-4) form pelvic nerve, and along with sympathetic nerves (T10-12) form pelvic plexus 3-4cm behind and to side of bottom of bladder and prostate, which gives rise to erigentes nerve (passing into corpus cavernosum). Somatic nerves (S2-4) form pudendal nerve (accompanying internal pudendal vessels, which arise from hypogastric vessels and themselves give rise to perineal and common penile arteries) and also give rise to dorsal nerve of penis and perineal nerve.
Physiology
The 2 corpora cavernosa (and to lesser extent the corpus spongiosum) inflate/fill with blood on arousal, and in so doing exert pressure on veins, reducing venous flow until progressive penile engorgement/erection/stiffness/turgidity causes a venous stretching and opening, and equilibrium of arterial and venous flow is reached in an erect state.
The external sphincter muscle of urethra (striated, ordinarily voluntary) surrounds (membranous) urethra in root, above/proximal to the ejaculatory ducts, and is prevented from relaxation during erection, by higher centres in brain, thus blocking sperm from the bladder.
Clinical
Peyronie’s disease (chronic inflammation of tunica albuginea, often with scar tissue formation and restricted erection, pain, shrinkage/deformity) affects up to 10% (of whom 30% also have other connective tissue problems such as Dupuytren’s contracture).
A lot of nerves courses near prostate and membranous urethra, prone to damage during related surgery, potential complications include impotence. Whereas most male mammals have an erectile bone (baculum) and can withdraw the penis into the abdomen, the human penis stays external and owes erection to engorgement with blood.
Interested in taking our award-winning Pocket Anatomy app for a test drive?